Treatment of Abdominal Aortic Aneurysms
What are the treatments for an abdominal aortic aneurysm (AAA)?
Your general health as well as the size and location of your AAA will determine how your aneurysm is treated. If your AAA is not big enough to need surgery straight away, your doctor may recommend an ultrasound or computed tomography (CT) scan every 3-12 months to carefully monitor the aneurysm’s size and shape. Your doctor may also prescribe certain medications to help keep the aneurysm stable, such as blood pressure medication and, if you smoke, you will be advised to stop. If your doctor feels there is risk that the aneurysm may rupture, surgical repair may be recommended. An AAA may be treated with either open surgical repair or by less invasive endovascular – or keyhole - repair techniques.
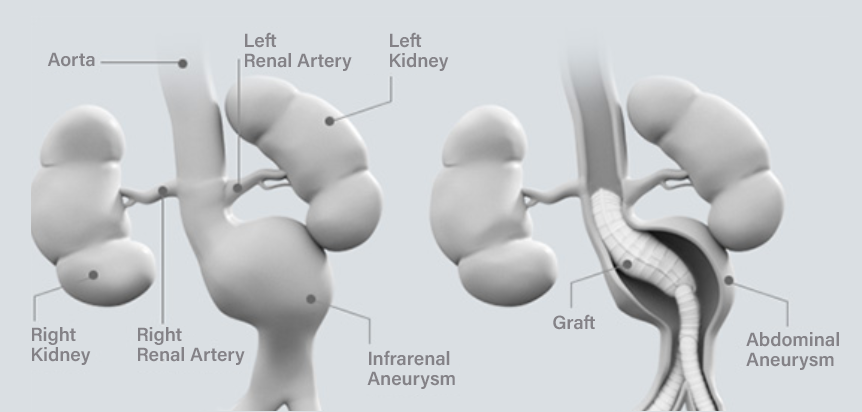
Open surgical repair
Your surgeon will open your abdomen to gain access to your aorta and then implant a graft into the weak area of your aorta. Blood will flow through the graft inside your aorta instead of going through the aneurysm, and this will prevent the aneurysm from enlarging further.

Endovascular aneurysm repair (EVAR)
Endovascular repair of AAAs is much less invasive than open surgical repair. The procedure involves placing a wire reinforced fabric tube graft (called a stent graft) inside your aorta which protects the AAA from blood pressure stress. Through small incisions in your groins, your physician will insert the stent graft parts over a guide wire. The graft is pushed through your femoral arteries and into the aneurysm by sliding along the wire. The stent graft is held in place through the use of metal hooks acting as anchors.
What are the possible risks of EVAR?
Not every patient is suitable for EVAR; the risks and benefits of both open surgical repair and endovascular repair procedures should be thoroughly discussed with your doctor. Following your endovascular repair, it is important that you have regular scheduled follow-up appointments with your doctor. Most common complications can be identified early with a CT scan or X-ray.
- Endoleaks – An endoleak is the leaking of blood around the repair into the aneurysm. Endoleaks can be detected using CT scans. Many endoleaks do not require treatment. Your doctor can decide if you need any treatment
- Stent graft movement – This is the movement of the stent graft from its original position over time. This can be assessed using imaging techniques like CT scans. Your doctor can decide if you need any treatment
- Device-related issues (for example, breaking sutures or the metal portion of the stent graft) – These issues may be detected using imaging techniques such as X- rays. Your doctor can decide if you need any treatment
- Endovascular devices require fluoroscopy and use of dyes for imaging. Patients with kidney problems may be at risk of kidney failure due to the use of dyes
- A hole or a tear of the blood vessels are risks associated with any catheter-based procedure
- Bowel complications including death of a portion of your bowel tissue requiring surgical removal
- Cramping pain and weakness in the legs, especially the calves
- Formation of blood clots that block the flow of blood to your organs
- Problems affecting your urinary and reproductive organs including infection and tissue death
What are the benefits of EVAR?
There are a number of benefits to having an EVAR rather than undergoing open surgery. Some of these are listed below:
- The procedure is minimally invasive, meaning that you do not have a large incision in your abdomen
- The procedure can be performed under local anesthesia, meaning that you can recover more quickly
- There is a lower surgical complication rate.
- There is a less risk that you will lose blood during the procedure, which reduces the risk of needing a blood transfusion
- You may spend less time in the intensive care unit after the procedure, and have a shorter hospital stay














